BLOG
Understanding Pelvic Girdle Pain (PGP) During Pregnancy
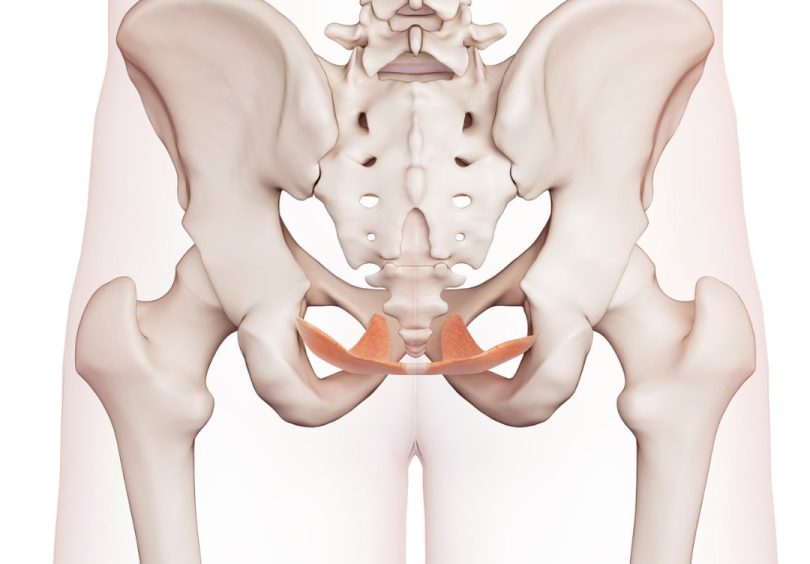

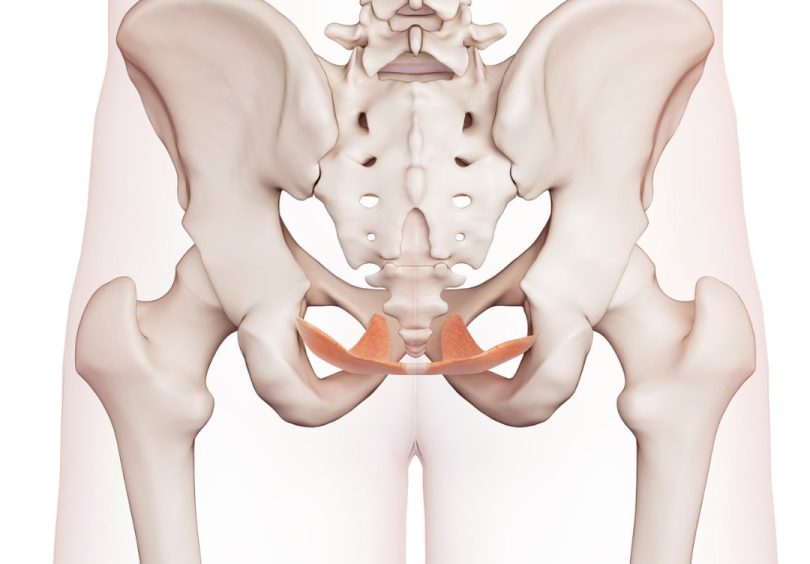
Pelvic girdle pain is a pain in the tailbone area (sacroiliac joints) and/or the front pubic bone (pubic symphysis) that is often felt in activities such as walking, rolling in bed and standing on one leg. Pain may radiate into the bottom or legs. Discover the causes and management of pelvic girdle pain (PGP) during pregnancy below.
33-50% of women will report pelvic girdle pain (PGP) before 20 weeks and 56-72% of women will report some degree of pelvic girdle pain by late pregnancy. PGP most commonly appears around 14 -30 weeks. The good news, in 93% of women, it settles within a few weeks of delivery.
The cause of pelvic girdle pain is multifactorial. There’s a growing understanding that it’s a complex mix of biological, psychological and social factors. PGP occurs because of several factors, including increased tissue sensitivity in pregnancy, changing load on the joints, fears around pain in pregnancy and well-meaning but often negative messaging about exercise and the safety of movement in pregnancy.
Whilst pregnancy results in an altered centre of gravity and increased lumbar lordosis (arch of the lower back), these postural adaptations are not linked with PGP. Hormonal, biomechanical and genetic changes, on the other hand, have been shown to play a role. More recently, a link has been shown between confidence in your body and fear avoidance behaviours play a significant role in PGP.
Although hormonal factors are thought to play a role in altered pelvic joint mobility during pregnancy, relaxin is no longer thought to be the primary hormone influencing this change. We now know that the relaxin hormone produced during pregnancy does not make the ligaments stretchier/looser and that the small amount of movement within the pelvic joints does not cause inflammation.
Oestrogen receptors exist in our soft tissues, such as muscles and ligaments. Throughout pregnancy, there is a shift of collagen fibre types in our joints due to the increase in oestrogen, which can impact the mechanical properties of the connective tissue.
The relationship between pain and increased range of motion is not linear. The pelvis remains incredibly stable, even in the presence of pelvic girdle pain. The increased sensitivity of the tissues drives the pain, and reduced muscle strength due to the pain, which gives the feeling of being less supported.
The risk of developing PGP increases with gestational age, a history of low back or hip pain, previous PGP or a family history of PGP, pelvic trauma, smoking and, interestingly, a lack of belief that PGP will get better.
Pelvic Girdle Pain can have a significant effect on both physical and mental health. It can lead to:
Difficulty performing daily tasks
Potentially impact the ability to work, resulting in social isolation
Feeling exhausted or powerless
Worry about safety issues with other children (e.g. not being able to run after toddlers)
Despite this, only 25% of women are referred for treatment. We are here to spread the word and change that statistic.
Given the causes of pelvic girdle pain are multifactorial, so too are the treatments. Understanding the pain and reframing beliefs can be helpful first steps to managing pain’s impact on daily living.
Outside of an acute injury (e.g. sprained ankle or burnt finger), pain is not a sign of damage or harm. It can give more of an indication of the sensitivity of the area. It is a messaging system that can be ‘upregulated’ (pain gets stronger) or ‘downregulated’ (pain gets reduced) by various factors. For example, if a tiger was chasing you and hurt your foot, even though this is an acute injury, your body downregulates pain because running away from the tiger is more important for survival. An example of upregulation is someone who has long-standing back pain and has had a poor night’s sleep. Because they are tired, they might feel sorer in their back, even though there has been no change to the bones/muscles of their back.
Keeping this in mind can help to reframe unhelpful thoughts such as “all pain is bad” and provide confidence that your body is robust and adaptable. The belief that PGP will go away is a strong predictor that it will go away!
When you feel like your pelvis is out of alignment, it usually reflects muscle tension that gives the perception that you are lop-sided.
Exercise improves well-being and reduces tissue sensitivity by teaching the brain that movement isn’t harmful and the pain isn’t dangerous or feared.
It is okay to exercise with discomfort in your pelvic joints. We don’t want you pushing into strong (>5/10) pain, or sharp pain that takes your breath away.
Pregnancy guidelines recommend at least 150 minutes of moderate-vigorous exercise per week.
If you have been doing an activity before you were pregnant, then it is generally safe to continue into your pregnancy. Some activities are recommended to stop or modify at various stages in your pregnancy, so if you are unsure, please speak to your Women’s Health Physio/Obstetrician/GP/Midwife.
If you experience any vaginal bleeding, stop exercising and review with your doctor/midwife before recommencing.
We here at Malvern Physiotherapy Clinic can help guide you through specific exercises that focus on the deep abdominals and muscles around the hip that provide dynamic stability to the pelvis. Unfortunately, this is not an instant fix. It can take six weeks to see changes.
Massage/Myotherapy
Support garments (tubigrip, tights, belts)
Taping techniques
Advice regarding ice vs. heat
Guidance on avoiding unhelpful movement patterns
Sleeping well, relaxing, and regular exercise will help
Minimise single-leg activities
Sit down to put pants on
Feet together to get out of the car
Stairs one at a time if necessary
Give yourself some horizontal rest
Minimise standing/ walking for prolonged periods
Wear low-heeled shoes
Minimise excessive loading e.g. lifting of heavy items or repetitive tasks.
Take breaks, change positions, or stretch for a few minutes.
Eat nutritious foods and make you feel good, and aim for adequate hydration (1.5-2L total fluid intake per day)
Encourage toddlers to climb onto a chair to be picked up where possible or sit down for a cuddle – of course, we understand this can be easier said than done!
Don’t let pelvic girdle pain limit your daily activities any longer. Schedule an appointment today and take the first step towards better health. Call us now at 9078 8434 or visit our website to learn more about our services and book online. We look forward to helping you on your journey to recovery.
Published February 21, 2024