BLOG
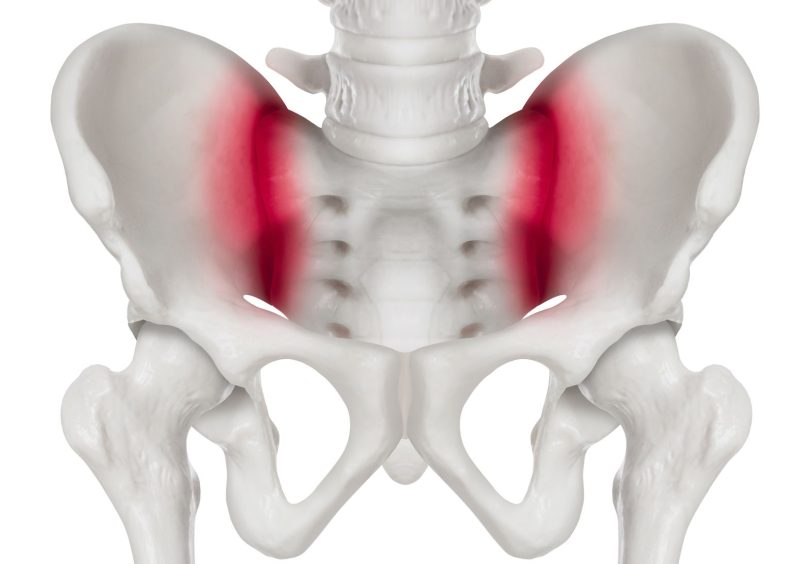
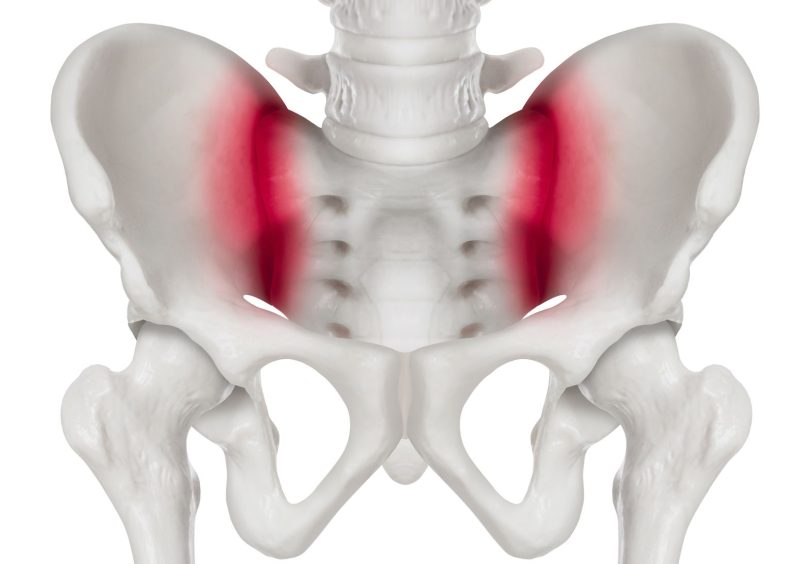
Pelvic Pain

This blog is the second in a series from Hayley Runting regarding pelvic health conditions. Today’s blog discusses pelvic pain, pelvic surgery and pelvic floor checks.
Pelvic pain can literally be a pain in the butt! However, it can also be defined as any pain in the pelvis or genital areas. There can be many causes of pelvic pain, such as trauma to the area, infection, or conditions like endometriosis. Working out what the contributing factors or the cause of the pelvic pain directs where treatment is focused.
There are two broad categories of pelvic pain – chronic pelvic pain and sexual pain (female and male):
Persistent pain in the pelvis region for greater than 3-6 months. This may involve muscles that attach into or out of the pelvis. There can be many different causes and reasons why someone has pain ongoing past normal tissue healing time frames. Individual assessment and management of the factors tailored to each person is the core of treatment.
Pain with penetrative intercourse or the inability to achieve penetration. Common conditions and terms you will hear include: vaginismus, vulvodynia, dyspareunia, and apareunia.
New terminology you may hear instead includes Genito-pelvic pain/penetration disorder (GPPPD) which encompasses both vaginismus, apareunia and dyspareunia. While it is called sexual pain, these conditions can also be related to pain with using tampons, tight fitting clothing or riding bikes.
Sexual Pain (Male): Pain with erections or ejaculation either in the penis, the testes or the perineum (area between the penis and the anus).
Both chronic pelvic pain and sexual pain can overlap, and both are often related to tight pelvic muscles and sensitised nervous systems after being sore for prolonged periods. Treatment focuses on incremental desensitisation, learning to relax pelvic floor muscles and breathing techniques to help manage or reduce the pain.
Pelvic surgery has been in the media a lot in recent years. While pelvic mesh has been shown to be adverse for prolapse pelvic surgery, alternative surgeries themselves can be very beneficial.
Pelvic and vaginal surgery, including hysterectomy (removal of the uterus), can be performed for various reasons. Prior to surgery, optimising your muscle strength, knowing how to manage pain, toileting and suitable exercises for the post-operative period is very beneficial. This also applies for men who are having prostatectomy surgery.
After surgery, recovering well from the beginning can set you up for good long-term outcomes. Knowing how to manage things such as constipation, heavy lifting, high-impact exercise and reduced pelvic floor muscle function are important. Occasionally after surgery men and women can experience problems such as bladder leakage or painful sex.
A pelvic floor physiotherapist and your surgeon can advise you on what will be best for your individual circumstances.
Individuals, although women in particular, are always encouraged to have their pelvic floor muscles assessed, even if they are not experiencing any symptoms or issues. Knowing how to correctly contract the pelvic floor muscles, receiving tailored exercises, and undergoing prevention screening is invaluable. It is also highly recommended to be assessed by a pelvic floor physiotherapist if you are unsure of how to do a pelvic floor contraction or feel that your muscles are weak.
This is particularly relevant for women who have recently had a child. A pelvic floor check is invaluable and can ensure that postnatal recovery is on the right track. For women who are keen to return to high-impact sport, ensuring the pelvic floor is working optimally is important to reduce the risk of incontinence or prolapse – both now and in the future.
This article is written by Hayley Runting, Physiotherapist.
If you would like any more information, or to book an appointment, please click the link or contact us on 9078 8434 or reception@malvernphysio.com.au
Published March 12, 2021